Items, providers, and other people merely can not get to the place they’re wanted with out efficient logistics. Logistics are important to just about all elements of the financial system and nationwide safety. Regardless of this, numerous challenges can disrupt logistics from extreme climate and international pandemics to distribution bottlenecks. On this weblog publish we’ll deal with cyber assaults to logistics determination fashions.
Nationwide safety and army organizations take into account contested logistics as “the atmosphere wherein an adversary or competitor deliberately engages in actions or generates circumstances, throughout any area, to disclaim, disrupt, destroy, or defeat pleasant power logistics operations, amenities, and actions.” For instance, in World Battle II, the Allied Transportation Plan included strategic bombing of main highway junctions, bridges, tunnels, rail strains, and airfields to hamper German actions to the Normandy space. This performed a decisive function within the success of the D-Day landings.
Whereas defending the bodily parts of logistics operations is vital, fashionable logistic programs additionally embody in depth software-based determination assist that’s important to logistics planning phases, and this software program additionally should be shielded from assault.
Past common cybersecurity, there are not any normal strategies for monitoring, detecting, and stopping cyber assaults to logistics determination fashions. Nonetheless, there are well-studied adjoining fields comparable to synthetic intelligence (AI) safety, machine studying operations (MLOps), and extra broadly AI engineering that may contribute to the securing of our logistics determination fashions.
Hypothetical Assault to a Logistics Mannequin
Take into account a logistics mannequin that determines distribute provides to hurricane victims in Florida. We have to resolve the place to find provide storage amenities, in addition to how provides from every facility are to be distributed to surrounding populations.
Within the context of nationwide safety and army operations, situations would possibly embody designing logistics programs to move gasoline, munitions, gear, and warfighting personnel from their originating areas to the entrance strains of a battle. One other army use case may be figuring out the optimum routing of autos, ships, and airplanes in a means that minimizes casualty threat and maximizes mission effectiveness.
Determine 1 illustrates utilizing a variation of the okay-center formulation to compute an optimum coverage for the Florida hurricane situation (left panel). If a cyber-attacker had entry to this mannequin and was in a position to modify its coefficients, then we would find yourself with a plan comparable to depicted in the suitable panel. The really useful central facility location has modified, which might degrade the effectivity of our hypothetical system, or worse, forestall catastrophe victims from receiving wanted provides.
In a army battle, even seemingly refined adjustments like a really useful facility location may very well be enormously damaging. For instance, if an adversary have been to have some functionality to assault or degrade a specific location unbeknownst to the defender, then manipulating the defender’s determination mannequin may very well be a part of an effort to bodily injury the defender’s logistics system.

Determine 1: Hypothetical instance of how a cyber attacker would possibly subtly regulate mannequin parameters in such a means that the mannequin recommends suboptimal or in any other case unfavorable insurance policies.
In follow, logistics determination fashions could be extraordinarily giant. For instance, the small linear mannequin used for Determine 1 solves a system of 266 pages of linear equations, which Determine 2 depicts. If 100 areas must be lined, the mannequin would have about 20,000 determination variables, about 40,000 constraints, and as much as about 800 million coefficients. Because of the drawback of scale, practitioners usually use approximation algorithms that may generate moderately good insurance policies for his or her particular issues.

Determine 2: System of linear equations (266 pages) required to generate the optimum coverage in Determine 1. Realistically sized fashions are considerably bigger, and it will be straightforward for refined mannequin manipulations to go undetected.
There are various varieties of logistics issues, together with facility location, automobile routing, scheduling, machine project, and bin packing. Logistics issues are sometimes formulated as linear applications. Determine 3 exhibits the overall type of a linear program, which (1) minimizes an goal operate (the vector of goal coefficients, c, multiplied by a vector of determination variables, x); (2) topic to a set of constraints (the constraint coefficient matrix, A, multiplied by the vector of determination variables, x, is the same as the constraint necessities vector, b); and (3) with the choice variables, x, taking up constructive values. Most logistics issues contain a variation of this mannequin referred to as a blended integer linear program, which permits a few of the determination variables to be integer or binary. For instance, a binary determination variable would possibly symbolize whether or not to open a provide depot (one) or not (zero) at a given location. Word that Determine 3 is a compact (small) mannequin illustration, and its use of vectors and matrices ( c, x , b , and A ) can mannequin any sized drawback (for instance with hundreds of determination variables, tens of hundreds of constraints, and tens of millions of coefficients).

Determine 3: Basic type of a linear program
George Dantzig invented the simplex methodology in 1947 to resolve linear applications, that are so pervasive that the simplex methodology is taken into account one of many nice algorithms of the twentieth century. Within the early 2010’s, it was estimated that 10-to-25 % of all scientific computation was dedicated to the simplex methodology. Right this moment, even with computing developments, fixing linear applications at-scale stays an unlimited problem.
In logistics follow, these fashions could be large. Not solely are they very tough to resolve, however they are often bodily unattainable to resolve with present computing know-how. Right this moment, a lot of the operations analysis subject is dedicated to growing approximation algorithms that yield top quality (though not essentially optimum) options to real-world logistics issues. Latest analysis (see right here and right here) supplies examples of such approximation algorithms. As a result of these mathematical applications are sometimes NP-hard (i.e., the issue measurement grows exponentially, and optimum options can’t be generated in polynomial time), optimization is among the promising use circumstances for quantum computing.
Discrete occasion simulation and system dynamics are additionally modeling kinds used to resolve logistics issues. Whereas we focus on linear programming as an exemplar mannequin kind on this weblog, different mannequin kinds could be equally susceptible to cyber assaults.
Idea of Operations
There’s little printed analysis, and even working expertise, concerning cyber assaults on logistics determination fashions. An assault would require undetected community intrusion; persistence to permit reconnaissance on the goal mannequin and assault planning; adopted by mannequin or knowledge manipulations which might be adequately subtle to be undetected whereas strategic sufficient to be damaging.
In follow, a profitable assault would require a classy mixture of abilities seemingly solely obtainable to motivated and skilled risk teams. Such risk teams do exist, as evidenced by intrusions into U.S. vital infrastructure and know-how enterprises like Google.
The Cyber Kill Chain developed by Lockheed Martin is a 7-step mannequin of how refined cyber assaults are sometimes carried out. The seven steps are: reconnaissance, weaponization, supply, exploitation, set up, command and management, and eventually appearing on the attacker’s targets. Attacking a call mannequin would equally require these steps to ascertain a persistent community intrusion, entry to the mannequin, and eventually manipulate the mannequin or its output.
As soon as attackers acquire entry to a logistics mannequin, the injury that they’ll inflict is determined by many components. Like AI safety, a lot is determined by the kind of entry gained (e.g., mannequin read-only entry, mannequin write entry, coaching knowledge read-only entry, coaching knowledge write entry, means to exfiltrate a duplicate of the mannequin or knowledge, and so on.). In contrast to many AI functions, logistics usually introduces sprawling provide chains of contractors and subcontractors. If an higher echelon determination mannequin is determined by knowledge from organizations at decrease echelons within the provide chain, then the mannequin might conceivably be attacked by poisoning knowledge in programs past the mannequin operator’s management.
Suggestions for Securing Logistics Determination Fashions
We name on the logistics, cybersecurity, and operations analysis communities to systematically examine the susceptibility of determination fashions to cyber assault and to offer formal suggestions for a way greatest to guard these fashions.
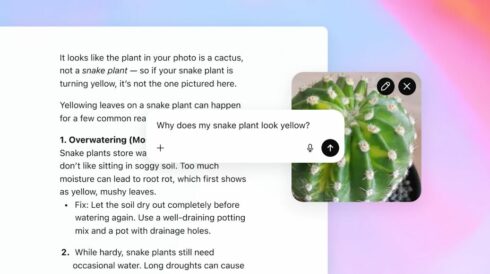
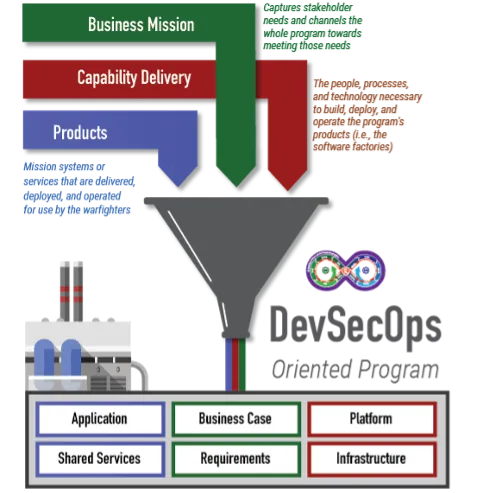
Within the meantime, there are well-studied adjoining fields that provide present logistics mannequin operators alternatives to enhance safety. For instance, machine studying operations (MLOps) is a scientific framework for making certain dependable deployments into manufacturing environments. Extra broadly, the SEI is main the Nationwide AI Engineering Initiative, which systematizes what is required to develop, deploy, and keep AI programs in unpredictable and chaotic real-world environments. Monitoring is a central tenet of MLOps and AI engineering, together with strategies to establish important mannequin and knowledge adjustments between revisions.
Lastly, we suggest that AI safety organizations take into account logistics determination fashions inside their purview. The linear programing that underpins logistics fashions shares many attributes with AI: each could be huge scale, compute intensive, depend on knowledge, and be tough to interpret. Like AI, assaults to logistics determination fashions can create important, real-world injury.